 Digitising health records has been a government goal since the days of the failed NHS National Programme for IT (NPfiT) – launched in 2002 with a budget of £6.2 billion its goal was, among other top-down changes, to introduce a nationally recognised, integrated electronic patient record (EPR) system to provide better visibility and transparency of patient care.
Digitising health records has been a government goal since the days of the failed NHS National Programme for IT (NPfiT) – launched in 2002 with a budget of £6.2 billion its goal was, among other top-down changes, to introduce a nationally recognised, integrated electronic patient record (EPR) system to provide better visibility and transparency of patient care.
It was officially ‘dismantled’ £13 billion later (some observers suggested the final bill was nearer £20bn) in September 2011. At the time it was considered the world’s largest civil IT programme, and its failure has been a subject of much discussion ever since.
Last month, Chancellor Rishi Sunak announced an extra £5.9 billion for the NHS in the Budget, of which £2.3 billion will be allocated to funding more diagnostic tests, £1.5 billion will be allocated to beds, equipment and facilities, and £2.1 billion will go towards improving IT and digital technology within the NHS.
Given the costs of such projects the last time around, one has to question whether this will be anywhere near enough. And, many in the medical community have already called for greater clarity on specifically what the money is to be spent on.
Back in the summer of 2020, we projected forward and predicted that more funding for NHS systems and digital transformation was not only desperately needed, but strongly expected in the 2021 budget in our article NHS – will this pandemic re-emphasise funding for its systems? 8 steps to ensure fit for purpose procurement. However, such investments often come with a healthy amount of measured anxiety as 50–70% of all complex IT projects, such as EPR, fail to succeed.
What is clear, from the lessons we have learned from the PR disasters that follow such projects, is that it’s often much more cost-effective to invest a little more in doing certain tasks upfront, than to pay (in all senses of the word) for all the remedial work required to clear up the misunderstandings over expectations and requirements afterwards. One example of which would be the day King’s College Hospital had to send a waiting room full of outpatients home after its EPR systems failed.
What is an Electronic Patient Record (EPR)?
An electronic patient record is a digitised version of an individual’s paper medical record, alongside a whole host of other information about them – immunisation status, lab test results, personal statistics, billing information and suchlike. This information, which is collected for all patients, can be used to provide better and more targeted healthcare for the individual, and collectively to provide the data needed to deliver care more efficiently and effectively to the population and to assist in the creation of new treatments and techniques.
What is an EPR system?
The collective digitised health records of a population are securely stored in an EPR system allowing for improved workflow efficiency, safety checks, prompts and so forth. The EPR system can also be linked to other NHS systems (e.g. drug prescribing systems, GP systems, community health systems) and hospitals. The benefit to the patient means they can attend any hospital as their full health record will be available for doctors to access, including medication, consultation history, scan images, etc. Having a full record for healthcare professionals minimises the risk of something important being overlooked and compromising the care provided.
What does a good EPR outcome/system look like?
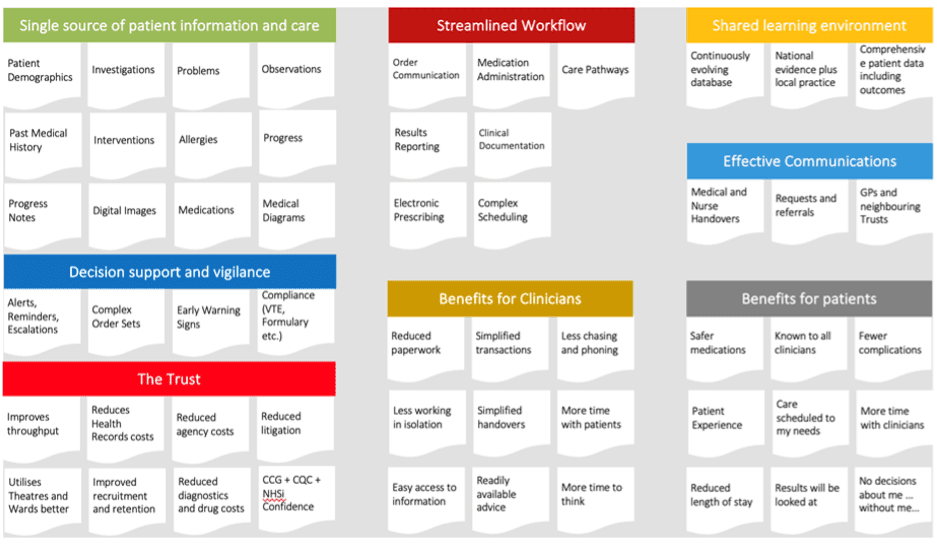
The implementation of a good EPR system in a hospital will likely offer streamlined workflow, greater decision support and vigilance, more effective communication between all relevant parties, a single source of patient information and care, plus a whole host of benefits for patients, clinicians and the Trust. We’ve summarised what ‘good’ looks like in a neat graphic below. However, it’s important to note that this is still just an overview of what will be a complex and wide-reaching project, the intricacies of which will necessitate adaptation to your specific circumstances through the use of SMART objectives.
What good ‘looks like’ For EPR
Who are the main EPR system suppliers?
The following is a list of EPR system and software suppliers which are all NHS accredited:
-
- Allscripts Healthcare (IT) UK Limited
- Cerner Limited
- Dedalus (formerly DXC)
- IMS MAXIMS
- MEDITECH UK
- Nervecentre Software Ltd
- System C Healthcare Ltd
- The Phoenix Partnership Ltd – TPP.
Note that we are not endorsing any of the solutions above; this list is purely to give you some visibility of the major providers in the EPR field. All EPR suppliers have their own idiosyncrasies in terms of how you procure from them and their strengths and challenges during the implementation process. The steps detailed below will help you capitalise on their strengths and minimise potential challenges during the procurement and implementation process.
11 Steps to successful EPR procurement and implementation
Realising the benefits of an effective, efficient and successful EPR system is a significant undertaking. From our years of experience in this arena, we can summarise the process of procurement and implementation into eleven defined steps, as follows:
Step 1 – The ‘Should Cost’ model
Understanding ‘whole life costing’ is important as part of your business case. Unrealistic expectations here (i.e. cost assumptions that are too low across the lifetime of the project) will likely cause funding issues further down the line. Creating a detailed cost model can help you to develop more productive collaborative working relationships, something we investigated in our article 5 steps to structuring a ‘Should Cost Model’ for strategic supplier services.
-
- As part of whole life costing, you need to identify all the cost areas not just the cost of the system. The following cost areas should form part of your whole life cost and ‘Should Cost Model’.
- Programme and Change Management. This includes initial project and programme management resources, change management resources, implementation phase such as data cleansing and migration, and training for all staff.
- Procurement. Too many business cases look at costs only from the point of contracting with a supplier and system implementation. They ignore the costs involved in ensuring the procurement process is fit for purpose. This is the work needed to ensure that:
- the right requirements, objectives and outcomes have been captured,
- that they have been properly articulated to the marketplace via Early Market Engagement, so suppliers have a chance to ask the right questions,
- they have an opportunity to undertake pre-contract due diligence,
- and that your contract is structured to drive the right behaviours between both you and the EPR solution provider.
- As part of whole life costing, you need to identify all the cost areas not just the cost of the system. The following cost areas should form part of your whole life cost and ‘Should Cost Model’.
The single biggest cause of disputes is misunderstandings over requirements (85%). Invest properly in the process to clearly articulate your expectations and requirements in advance of the procurement process.
-
-
- Infrastructure. While software will be part of the supplier’s cost, where you anticipate using a legacy model of on-premise installation (on-site), you might need to upgrade your desktops, tablets, operating systems and servers. Where a public or private ‘cloud-based’ or Infrastructure as a Service (IaaS) is involved, then server response time and communications bandwidth are often key constraints. As part of a structured due diligence process to be undertaken by potential suppliers, ensure that they carry out an appropriate due-diligence exercise on your ‘as is’ infrastructure and ask them to identify if your current set-up is fit for purpose. If it’s not, ask them to suggest what improvements are needed.
- Estate/facilities. Where will you accommodate the team and where will training occur? Do you need to involve your estate suppliers? Is there a cost involved for installing computers, e.g. for PFI hospitals?
- Contract and Supplier Management. Internal contract management costs and IT service management costs.
-
Step 2 – Clear expectations
Knowing what you want to achieve and why is vital to the process. Understanding the issues your solution should address and the real-world practical ways in which these issues limit frontline workers from delivering at their best, alongside the specific ways in which your solution will change things, is fundamental to the success of the project.
Clarity in expectations and objectives, in enough depth to feed the project machine, is not something that can be achieved quickly. Expect to invest 3 to 6 months into this process alone to achieve the clarity that both your internal stakeholders and the suppliers can agree and deliver on.
Step 3 – Clear objectives
Be specific with your supplier about the quantified objectives you wish to achieve with your solution or system. How else can either party identify whether or when those objectives – and each milestone on the road to your objectives – have been met?
This is not an easy process, and that truly is an understatement, but calculating the reasons to justify the expense you are about to commit to, and the challenges you’ll face, is a vital part of the process of offering clarity to all involved and to gain buy-in and support from all stakeholders to the project.
Step 4 – Focus on outcomes rather than features
EPR implementations should drive clinical and operational improvements in clinical processes. This is not a chance to simply translate what you’re doing into a digital form. It’s an opportunity for a deeper look under the hood of why clinical workflows and operational processes are undertaken – specifically focusing upon what works really well and where improvements can be made.
In one study, surgical clinic design, patient scheduling, physical space layout, staffing and workflows were all improved as a part of the ‘EPR implementation’ process.
A recent survey of more than 1,600 emergency care professionals suggests that good NHS EPR usability can benefit a hospital’s clinical, patient flow, and financial functions. It may actively prevent patient harm too, by enforcing clinical safety systems.
Step 5 – Strong stakeholder management
This should not be considered simply an IT project, but should instead be thought of as a business change project.
All stakeholders must be properly engaged with and consulted – especially clinicians and nurses. However, clinician availability can prove challenging, so this must be properly planned to ensure their engagement is high. People fundamentally dislike change; however, the perceived challenges and risks associated with this change can be minimised via effective communication and stakeholder management.
Organisational leadership has an important part to play here. Buy-in from the top is vital, but equally end users need to feel that they have been engaged with and considered in the decision-making processes.
Step 6 – Strategic supplier management
Successful EPR projects require a collaborative mindset and matching actions. Both the client and the supplier must deliver on their responsibilities within expected parameters (at the very least), or one will be holding the other back, dragged down by the weight of implementation failures.
Early identification of an imbalance in this dynamic is important. Allowing poor behavioural traits to go unchecked will encourage them to spread to others, exacerbating the problem still further.
Implementation issues in EPR solutions, to a lesser or greater degree, are inevitable. In complex EPR projects there are so many moving parts that at some point in the supplier relationship, the wheels will threaten to come off. It is then ‘how’ you handle the realignment of commitment, trust and behaviour that will make all the difference. Embodying the behavioural traits you wish to see in others is a good start, avoiding finger pointing and promoting greater commercial trust and collaboration is vital as strategic supplier management should be more about realignment than recourse.
Early indications that things may be about to go awry may go unnoticed, which is why it’s important to have a team dedicated to the goal of managing, monitoring and enhancing your supplier relationships, a team we call the Intelligent Client Function (ICF). They are a cross-departmental group of experts whose responsibilities include supplier insight, problem foresight and relationship development so issues can be avoided or resolved far more swiftly.
Step 7 – Aligned culture and support
Procurement often focuses a disproportional amount of effort on determining how well the strategic supplier responds to the bid, answering the question ‘are they able to do the job?’. However, just as important is the supplier’s culture and its alignment to your own – for example – what will working with them be like, how have they worked with other clients in the past, what is their own culture and how willing are they to support their clients in their goals?
A misalignment in both the supplier’s and client’s corporate culture can lead to all manner of issues along the way, which is why seeking evidence of alignment in this area is just as important at the procurement stage as your supplier’s technical capabilities.
Step 8 – Early market testing
This is a vital part of concept validation. Having internally agreed a degree of clarity on your expectations and Use Cases, go out to the market as early as possible to speak with expert suppliers in the field to determine whether your expectations are achievable and to gain a better understanding of the challenges you’ll face and how you might look to mitigate them.
Early market testing can also be used to identify whether your budget, schedule and objective expectations are realistic and can, therefore, contribute to the shape of the procurement process going forward for a fit-for-purpose solution.
For a free early market testing guidance document, including what questions to ask expert suppliers, click here.
Step 9 – Evaluating and scoring tenders
The creation of an evaluation framework is incredibly important for two foundational reasons:
-
- So you have a true and fair way of comparing the relative strengths of all those who submit tenders in your procurement process, and
- So you have the mechanism to provide complete clarity and transparency in the way you score tenders to make it more difficult for your process to be challenged either by internal stakeholders, or if you are in the public sector, by your suppliers.
The creation of a bespoke evaluation framework is a highly complex task and, for public sector readers, one that has its own article (it also has some highly salient points for private sector readers, too). If you wish to investigate the step-by-step process for yourself, look at How to create an evaluation framework for procurement tenders.
Step 10 – Create a fit-for-purpose ‘enabling contract’
Your contract is your guide for what will often be a very long and complex relationship, therefore it’s important to draft it, 1) as a ‘live, operating’ document that governs your relationship, 2) with fairness, equity and realistic flexibility in mind, and 3) to consider it an ever-evolving document requiring regular realignment with the real-world changes in your relationship.
As you progress through the years on your project, and within your relationship, you’ll gain a better understanding of your strategic partner in the process, you’ll get to know their strengths and weaknesses, their capacities and their challenges. You’ll understand better what they respond to and what will trigger them.
You’ll want to build this into your agreement to achieve better results. The project’s environment will also change with technologies, trends, expectations and needs transforming over time. This, too, should be considered within your agreement, as KPIs will need to be amended to ensure that they are achievable and pull the parties towards expected outcomes.
Build in a biannual ‘review and refine’ (we call it ‘reshaping’) process into your contract so it can be assessed against real-world challenges and solutions that will make it more of a ‘living document’; one that can be agile to change and more likely to drive success ‘enabling’ behaviours. It also offers an opportunity to air issues that have limited productivity or pushed progress off the correct path.
Step 11 – Good contract and supplier relationship management
The management of your relationship is closely aligned with the management of your contract, as the mechanisms for guiding and informing parties all reside within its pages. At times, a realignment is needed and the agreement itself will need to be assessed against its capacity to achieve the outcomes expected from the relationship.
However, there will be times when it can be simply referred to and the implementation of its measures carefully considered against real-world knowledge of the methods of application, which may achieve the best response.
Good contract and supplier relationship management is another area with a significant opportunity for improvement in many strategic supplier relationships. For a deeper appreciation of the lengths you can go to in order to build stronger relationships through the way you approach your legal documents, take a look at our article on the subject 11 Tips for Good Contract Management Strategies to Drive Success in Major Projects.
How can we help with your EPR procurement or implementation?
If you are considering the business case, early market engagement, procurement and/or implementation of an EPR solution – or perhaps realigning an existing implementation that is not quite fulfilling your expectations, we have a great deal of expertise in this specific arena.
For access to a full suite of guidance and documentation, templates or to schedule a conversation about your specific challenges, contact us on 0845 345 0130 or at advice@bestpracticegroup.com

